
Understanding Low Back Pain: Insights from O’Sullivan’s 2005 Study
When I started researching chronic low back pain (CLBP), I was surprised by some findings. In particular, I didn’t realize it is a leading cause of disability worldwide. Allegri’s 2016 study, Mechanisms of low back pain: a guide for diagnosis and therapy, shows that the number of people with CLBP has more than doubled over the last decade, affecting adults across all ages and ethnicities. The condition comes with high costs due to healthcare expenses and lost productivity, emphasizing the need for effective management.
For individuals with scoliosis, managing low back pain can be even more challenging due to the way the spine curves. At ScoliosisPTJax, we use personalized care to address both the physical and emotional aspects of pain. A helpful tool we use is O’Sullivan’s (2005) model for mechanical low back pain (MLBP). This model categorizes LBP into specific types based on how people move, providing strategies to treat the whole person.
In this blog, we’ll explore O’Sullivan’s classification system, its relevance to scoliosis-related LBP, and how Pilates-based strategies can help manage pain effectively.
O'Sullivan's Classification System for MLBP

O’Sullivan’s (2005) study divides MLBP into groups to better match treatment to the problem. The groups are:
- Flexion-related dysfunction: Pain aggravated by forward bending.
- Extension-related dysfunction: Pain exacerbated by backward bending.
- Multidirectional movement control impairments: Pain from poor stability and control in various directions.
This system helps create specific exercises for each problem instead of using a general treatment plan.
Key Concepts from O'Sullivan's Study
1. Core Stability Focus
O’Sullivan’s study highlights the importance of enhancing core stability and improving motor control. Core stability involves not just strong superficial muscles (like the rectus abdominis or “six-pack” abs), but also the activation and coordination of deep stabilizing muscles, such as the transverse abdominis, multifidus, pelvic floor muscles, and diaphragm. These muscles work together to create a foundation for efficient movement and protect the spine from excessive stress.
Key Points:
- Superficial Strength vs. Deep Stability:
Strong outer abdominal muscles do not guarantee spinal stability. The deep core muscles must engage appropriately to stabilize the spine during movement. Without this engagement, inefficient movement patterns can lead to strain and pain. - Role of the Transverse Abdominis:
- Acts as a natural corset, stabilizing the spine by increasing intra-abdominal pressure.
- Crucial for maintaining a neutral spine during dynamic activities.
- Multifidus Activation:
- Provides segmental stability to the vertebrae, preventing excessive motion at individual spinal segments.
Exercises to Enhance Deep Stability:
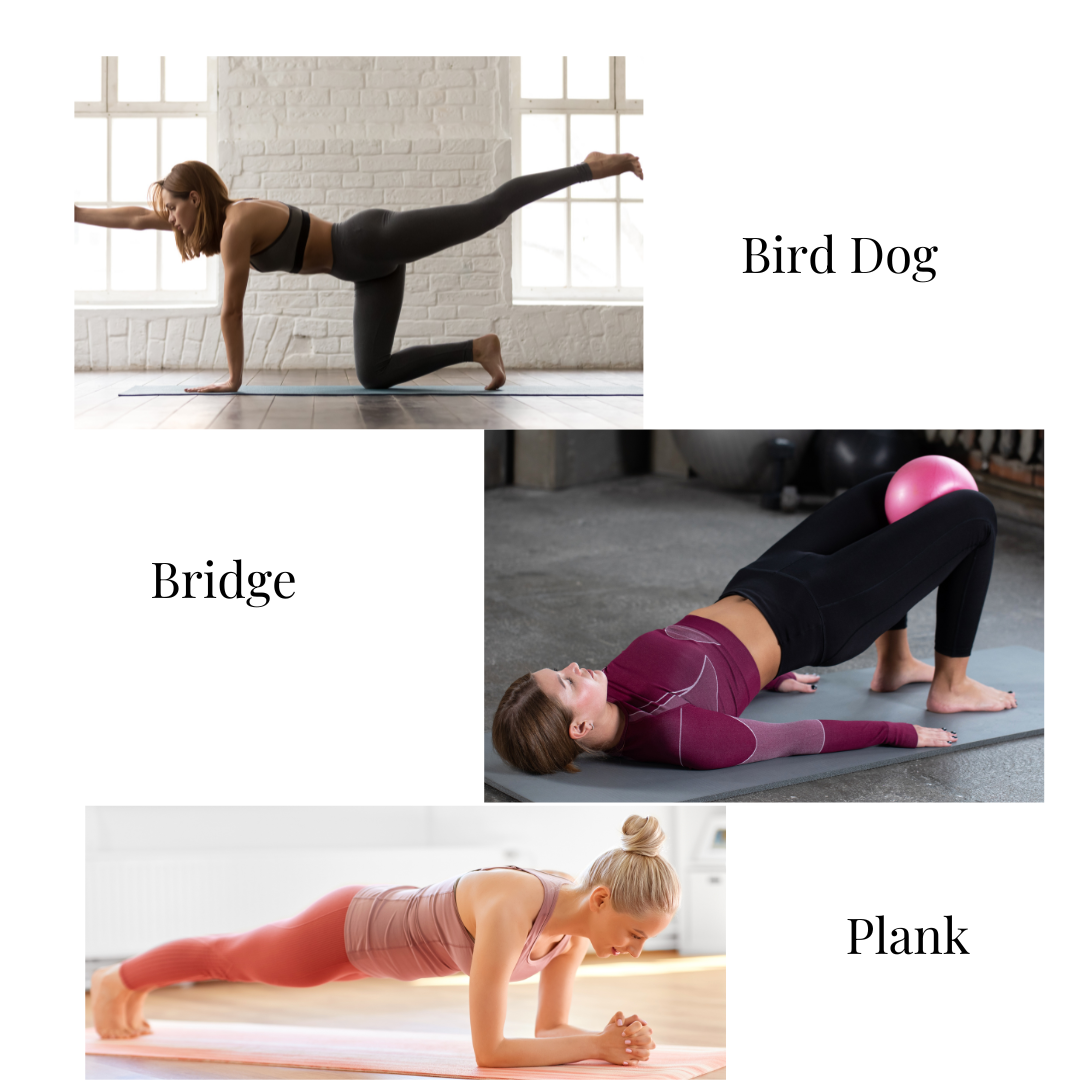
- Bird-Dog:
- Position: Hands and knees.
- Action: Extend one arm and the opposite leg while keeping your torso stable. Avoid arching or rotating your back.
- Tip: Imagine a cup of hot coffee on your back; don’t spill it. Repeat 10x.
- Bridging:
- Position: Lie on your back with knees bent, feet flat on the floor, and a ball between your knees.
- Action: Squeeze your glutes and lift your hips toward the ceiling. Lower hips slowly, repeat 10x.
- Plank:
- Position: Forearms and toes, body in a straight line.
- Action: Keep hips level and engage your core. Avoid sagging or piking hips.
- Tip: Hold for 20-30 seconds, increasing as you build strength.
Why Deep Stabilizers Matter:
Focusing on these muscles redistributes loads more evenly across the spine, reducing reliance on superficial muscles and minimizing compensatory patterns that lead to chronic pain.
2. Biopsychosocial Model
This model acknowledges that LBP is influenced by physical, psychological, and social factors.
Psychological Factors:
- Fear-avoidance behaviors: Avoiding movement due to fear of pain, leading to deconditioning.
- Stress and anxiety: Amplify pain perception and increase muscle tension.
- Patient beliefs: Misunderstandings about pain can hinder recovery.
Social Factors:
- Support from family, friends, or coworkers influences coping strategies.
- Work or lifestyle demands may contribute to chronic stress or poor movement habits.
Clinician Focus:
- Educate Patients: Provide evidence-based explanations and reassure that movement is safe.
- Address Fear-Avoidance Behaviors: Encourage gradual exposure to previously avoided movements.
- Incorporate Stress Management: Teach relaxation techniques such as diaphragmatic breathing or mindfulness.
3. Active Rehabilitation
Active rehabilitation empowers patients to take an active role in their recovery, emphasizing movement and self-management strategies.
- Active Rehabilitation: Builds strength, flexibility, and motor control to correct dysfunctional movement patterns.
- Passive Treatments: Provides temporary symptom relief but may foster dependency on clinicians.
4. Education and Self-Management
Patient education is key. Empowering individuals with proper movement strategies reduces dependence on healthcare providers.
Pilates-Based Strategies for Managing Scoliosis-Related LBP
Pilates emphasizes core strength, alignment, and control. Here are some examples:
- Plank:
- Issue: Pelvis drops unevenly or back arches.
- Modification: Hover plank on hands and knees; focus on pelvis level.
- Roll-Up:
- Issue: Uneven spinal articulation.
- Modification: Use a wedge or Pilates ball to support the lower back.
- Side Plank:
- Issue: Pelvic instability.
- Modification: Start with knee-down; progress as stability improves.
Practical Tips for Managing LBP with Scoliosis
- Get an Assessment: Identify primary issues like movement restriction or control impairment.
- Incorporate Props: Use towels, wedges, or Pilates balls for alignment and feedback.
- Focus on Quality Over Quantity: Perform exercises slowly and with precision.
- Address Psychosocial Factors: Include stress management techniques and patient education.
Conclusion
O’Sullivan’s 2005 study revolutionized MLBP treatment by integrating movement science with psychosocial considerations. For individuals with scoliosis, addressing movement dysfunctions and incorporating Pilates principles can significantly reduce pain and improve function.
Call to Action
Struggling with scoliosis-related LBP? Contact us for a comprehensive assessment and personalized care to improve your movement and quality of life.
References
- O’Sullivan, P. (2005). Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanisms. Manual Therapy, 10(4), 242-255.
- Allegri, M., et al. (2016). Mechanisms of low back pain: A guide for diagnosis and therapy. F1000Research, 5, 1530. https://doi.org/10.12688/f1000research.8105.1